About Celiac Disease
For most people, eating foods with wheat, rye or barley is natural and normal. Gluten is the common ingredient in all these foods. Gluten-based protein is an important part of the diet for billions of people around the world. For people with the inherited auto-immune condition called Celiac disease, problems occur when gluten gets ingested.
Along the walls of the intestines that are fingerlike projections called villi. The villi help to break down and absorb the food we consume. Within each villi are much smaller features called micro-villi. Small pieces of gluten flow past the villi and eventually, into the blood stream to nourish our bodies.
In people with the inherited auto-immune disorder called Celiac disease (CD), instead of viewing gluten as a nutrient, their bodies treat it as an invader, a threat to the body that needs to be attacked. Armies of immune cells are created which then release chemicals that harm the lining of the small intestine, flattening and even destroying the microvilli and the larger villi.
This reduces the bodies ability to properly absorb nutrients (malabsorption) and / or allows other molecules into the blood stream that healthy villi normally keep out (leaky gut.) As a result, a person with CD may experience obvious symptoms of digestive pain, constipation, diarrhea, and fatigue. Since these symptoms can be common to other conditions, people with CD are often misdiagnosed with irritable bowel syndrome, lactose intolerance, chronic fatigue syndrome, diverticulosis, ulcers or allergies.
Malabsorption of nutrients can also lead to less obvious problems like slowed growth and development in children, anemia, osteoporosis and fertility issues. People with celiac disease often suffer for years before a correct diagnosis is made. Sadly, more than 95% of Canada’s celiacs are not diagnosed in their lifetime and if they are, it will have taken an average of 12 years of visits to medical care providers. Celiac disease is estimated to affect 1 out of 100 people world wide.
If CD is undiagnosed or left untreated, it can lead to the possible development of a cascade of other autoimmune disorders. CD occurs at higher rates in individuals who also diagnosed with Type 1 diabetes, auto-immune thyroid disease, autoimmune hepatitis, Down syndrome and Turner syndrome. If a person has any of these disorders as well as digestive symptoms, or a family history of CD, a person should be screened for the disease.
When should you be tested for Celiac disease:
• abdominal pain, bloating and gas
• bone and/or joint pain
• canker sores
• chronic fatigue and weakness
• depression, lethargy, brain fog
• diarrhea, constipation or both
• easy bruising of the skin
• elevated liver enzymes
• indigestion/reflux (heartburn)
• infertility (in both women and men
• iron, folate and/or vitamin B12 deficiency
• lactose intolerance
• menstrual irregularities
• migraine headaches
• nausea and vomiting
• other vitamin and mineral deficiencies
• recurrent miscarriages
• swelling of hands and feet
• unexplained iron deficiency
• weight loss, although 30% of celiacs are above their ideal weight at the time of diagnosis
 Additional symptoms in children:
Additional symptoms in children:
• abdominal bloating and pain
• chronic diarrhea
• vomiting
• constipation
• pale, foul-smelling, or fatty stool
• iron-deficiency anemia
• weight loss
• fatigue
• irritability and behavioral issues
• dental enamel defects of the permanent teeth
• delayed growth and puberty
• short stature
• Attention Deficit Hyperactivity Disorder (ADHD)
• concentration and learning difficulties
• dental enamel abnormalities
• failure to thrive (delayed growth and short stature)
 Because CD is a genetically-mediated disease that can be passed on in families, it is important that when one person is diagnosed, that 1st degree (parents, children, siblings) and 2nd degree relatives (aunts, uncles, cousins, grandparents and grandchildren) should ask their doctors for the pre-screening blood test that detects the antibodies that are associated with CD.
Because CD is a genetically-mediated disease that can be passed on in families, it is important that when one person is diagnosed, that 1st degree (parents, children, siblings) and 2nd degree relatives (aunts, uncles, cousins, grandparents and grandchildren) should ask their doctors for the pre-screening blood test that detects the antibodies that are associated with CD.
What are the blood tests for Celiac disease*? 
There are two blood tests that measure the presence and quantity of ‘army’ of auto-immune cells that gluten triggers in individuals with CD:
• tTg: IgA anti-transglutaminase antibody test
• Total Serum IgA
While these blood tests are very sensitive, they are not 100% accurate. If the tTg test is positive or the IgA test shows a deficiency, a duodenal biopsy is required to make a definitive diagnosis. Collected under mild sedation, evidence of the damage that gluten creates in the microvilli and larger villi provides a definitive diagnosis. Printer-friendly version Blood Tests for Celiac Disease or click on the image below.
*Blood tests and intestinal biopsies are diagnostic services that are provided at no charge to residents of British Columbia. See Medical Services Plan.
 IMPORTANT: It is essential that the blood test and the biopsy be performed before removing gluten from your diet. Starting on the gluten-free diet prior to testing can interfere with making an accurate diagnosis. If you have already removed or reduced the gluten in your diet, medical experts recommend a gluten challenge, prior to both the blood tests and the duodenal biopsy.
IMPORTANT: It is essential that the blood test and the biopsy be performed before removing gluten from your diet. Starting on the gluten-free diet prior to testing can interfere with making an accurate diagnosis. If you have already removed or reduced the gluten in your diet, medical experts recommend a gluten challenge, prior to both the blood tests and the duodenal biopsy.
Adults – 10 grams of gluten (4 slices of bread or equivalent) for at least 1 month prior
Children – 5 grams of gluten (2 slices of bread or equivalent) for at least 1 month prior
If you have been on a gluten-free diet for a long time it may take 2-3 months on a gluten challenge to turn the tTg and biopsy positive. Because it can be very uncomfortable to reintroduce gluten to one’s diet, it is strongly recommended that you consult your medical care provider about being prescreened for CD BEFORE removing gluten from your diet. The gluten challenge is truly ‘a challenge.’
 Can I view my test results online?
Can I view my test results online?
Yes! My e-Health offers a fast and secure method for patients to receive their results electronically. As soon as results are released from the performing lab, they’re available online in my ehealth. Excelleris uses a variety of secure technologies and procedures to help protect your information from unauthorized access, use or disclosure. My ehealth is a free service and is available in 4 languages.
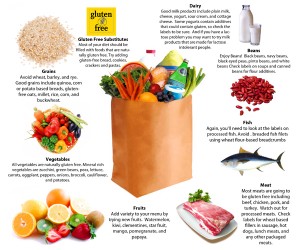
People with celiac disease can no longer eat foods with wheat, rye or barley and sometimes oats, too. The only effective treatment is a life long, strict avoidance of gluten-containing foods. Once on a gluten-free diet, the lining of the small intestine repairs itself and will remain healthy, provided one avoids eating any gluten, for life. Even a small amount of gluten – less than the head of a pin – can trigger a celiac’s immune system and create damage in the small intestine. A person may not be aware that their intestines are being affected so it is important not to use ‘outside’ symptoms as an indication of what may or may not be happening ‘inside.’ Always check labels, take care to prevent cross contamination when preparing both gluten-containing meals and gluten-free foods and ask questions when consuming food prepared by others.
What is Non-Celiac Gluten Sensitivity?
Individuals with Non-Celiac Gluten Sensitivity (NCGS) experience digestive symptoms that are similar to those experienced by individuals with Celiac disease. Like celiacs, their symptoms improve when gluten is eliminated from their diet. Unlike celiacs, their bodies do not create antibodies to gluten, nor do they exhibit the damage to the small intestine that is the hallmark of Celiac disease. People with NCGS are at no greater risk of developing additional autoimmune conditions or digestive cancers. At the moment, there are no tests that can prove whether one has NCGS. A diagnosis of NCGS can be made when tests for Celiac disease are negative. It is estimated NCGS affects 6-10% of the population.
 What is Dermatitis Herpetiformis?
What is Dermatitis Herpetiformis?
Dermatitis Herpetiformis (DH) is an inherited autoimmune disease of the skin marked by groups of watery, itchy blisters. Like Celiac disease, ingesting gluten triggers an immune system response that deposits inflammatory lgA antibodies under the top layer of skin. See Celiac Disease Has a Little Sister
The lgA deposits result in eruptions similar to the beginning of a pimple. This painfully itchy rash may progress to red, raised patches of skin that develop into small, watery blisters. The itching and burning of the eruptions are severe and the urge to scratch them is intense. Eruptions commonly occur on pressure points – around the elbows, the front of the knees, the buttocks, back, shoulders, face, and scalp and typically occur in parallel, on both sides of the body. Sixty percent of those diagnosed are men and the most common ages at diagnosis are between 15 and 40 years old.
A small biopsy of unaffected skin, next to an eruption that reveals the presence of IgA deposits confirms a diagnosis of DH. A strict gluten-free diet for life is the only treatment, but the diet should only be started once a diagnosis has been made. The medication Dapsone may be prescribed to ease symptoms until the gluten-free diet reduces the severity and frequency of eruptions.
Why can’t I just go gluten free? Why do I need to be tested?
Knowing whether or not you have a chronic autoimmune disorder is important to your future health and the health of your family. There may be a price for choosing not to know.
• Screening for Celiac disease is free in British Columbia
• Blood samples can be collected at your local out patient laboratory
• A diagnosis will tell you how strict your diet needs to be
• In conjunction with a lifelong commitment to the diet, health complications may be reduced
• Your doctor can better monitor your health for other autoimmune disorders
• Celiac disease is genetic. A diagnosis confirms for your family that they may also be at risk
• Familial screening provides an early diagnosis for those with latent (asymptomatic) Celiac disease
• A diagnosis offers eligibility for future therapies that require a definitive diagnosis
• You may qualify for a Medical Expense Tax Credit
• If Celiac disease is ruled out, your doctor can proceed to test you for other disease(s)