Do Changes in the Gut Microbiome Precede Celiac Disease?

- Megan Brooks; CME Author: Laurie Barclay, MD 1
Clinical Context
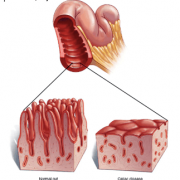
Celiac disease pathogenesis involves gluten exposure, genetic compatibility, and the gut microbiome, which may mediate interactions between gluten/environmental factors and the immune system. Mechanistic insight into pathogenesis of CD and other autoimmune diseases requires prospective longitudinal studies to examine subjects at multiple time points before disease development.
Study Synopsis and Perspective
Changes in the gut microbiome are present in infants at risk of developing CD long before they actually develop the disease, a finding that may pave the way for novel treatment and prevention strategies.
Researchers tracked shifts in the gut microbiota of 10 infants who developed CD and 10 matched infants who did not develop the autoimmune condition.
As early as 18 months before onset of CD, they observed increases in microbial strains, functional pathways, and metabolites previously linked to autoimmune and inflammatory conditions.
These preclinical changes in gut microbiota were present “much earlier than we expected,” lead author Maureen Leonard, MD, with the Center for Celiac Research and Treatment at Massachusetts General Hospital for Children (MGHfC), said in a news release.
If confirmed in larger datasets, the findings may aid in developing predictive biomarkers of onset and possibly provide novel therapeutic or preventive targets to intercept the disease before it sets in.
“With these findings, we anticipate that we will be able to distinguish who will remain healthy and who will develop celiac disease months before the onset of the disease,” senior author Alessio Fasano, MD, who is also with the Center for Celiac Research and Treatment at MGHfC, said in the same release.
The study was published online July 12 in Proceedings of the National Academy of Sciences.
Clinical Implications
- Distinct changes in gut microbiota precede CD onset in at-risk infants.
- The current study by Leonard and colleagues established a road map for prospective longitudinal study designs to clarify the role of gut microbiota in disease pathogenesis
- Implications for the Healthcare Team: The healthcare team should be aware that these findings may suggest novel therapeutic and preventive targets.
Early Gut Signature of Progression to Celiac Disease
Celiac disease is a chronic systemic autoimmune disorder that occurs in people genetically predisposed to the disorder. Dietary gluten acts as the trigger.
Alterations in the gut microbiota have been linked to CD as well as inflammatory bowel disease, type 1 diabetes, and multiple sclerosis.
As part of the MGHfC Celiac Disease Genomic, Environmental, Microbiome, and Metabolomic (CD-GEMM) study, researchers are tracking changes in gut microbiota of 500 infants at genetic high risk for CD from birth through age 10 years. They collect fecal samples every 3 months for the first 3 years after birth and then every 6 months until age 5.
In their article, the researchers reported on the 10 infants who developed CD and the 10 who did not. They focused on a time window spanning the 18 months before the time of onset to capture very early changes in the microbiome.
Longitudinal analysis of microbial species, pathways, and metabolites revealed “major shifts” in gut microbiota profiles and associated metabolomes before disease onset, they report.
For example, before CD onset, there was an increased abundance of several microbial species/strains/pathways/metabolites previously linked to autoimmune and inflammatory conditions: namely, Dialister invisus, Parabacteroides species, Lachnospiraceae, tryptophan metabolism, and the metabolites serine and threonine.
Others that are known to have anti-inflammatory effects occurred in decreased abundance before CD onset: namely, Streptococcus thermophilus, Faecalibacterium prausnitzii, and Clostridium clostridioforme.
The researchers also uncovered previously unreported microbes/pathways/metabolites that may represent CD-specific biomarkers: namely, Porphyromonas species, high mannose-type N-glycan biosynthesis, and serine.
“Our study establishes a road map for prospective longitudinal study designs to better understand the role of gut microbiota in disease pathogenesis and therapeutic targets to reestablish tolerance and/or prevent autoimmunity,” they wrote.
Study Highlights
- This longitudinal, prospective birth cohort study used metagenomics analysis of gut microbiota of infants at risk for CD to monitor microbiome shifts before CD development.
- 10 infants who developed CD and 10 matched unaffected infants underwent cross-sectional and longitudinal analyses of gut microbiota, functional pathways, and metabolites, starting from 18 months before CD onset.
- Cross-sectional analysis at CD onset identified altered abundance of 6 microbial strains and several metabolites between cases and control participants, but no change in microbial species or pathway abundance.
- Still, longitudinal analysis showed increased abundance of several microbial species/strains/pathways/metabolites detected before CD onset.
- These had previously been linked to autoimmune and inflammatory conditions, including Dialister invisus, Parabacteroides sp., Lachnospiraceae, tryptophan metabolism, and metabolites serine and threonine.
- Others, with known anti-inflammatory effects, decreased in abundance before CD onset, including Streptococcus thermophilus, Faecali bacterium prausnitzii, and Clostridium clostridioforme.
- Previously unreported microbes/pathways/metabolites suggesting CD-specific biomarkers included Porphyromonas sp., high mannose type N-glycan biosynthesis, and serine.
- The investigators concluded that their study established a road map for prospective longitudinal study designs to clarify the role of gut microbiota in disease pathogenesis, including potential causal links.
- The findings suggested that gut microbiota, functional pathways, and metabolome changes before CD onset may be used to predict disease and potentially to identify early preventive and/or therapeutic interventions to reestablish gluten tolerance and prevent autoimmunity.
- The identified alterations suggest progression from preclinical disease to a break of tolerance to gluten and subsequent CD onset.
- As CD is a model of autoimmune diseases, this approach could facilitate personalized prevention and treatment strategies for CD and potentially for other autoimmune conditions.
- The findings identified complex patterns of increased abundances of proinflammatory species previously linked to inflammatory and autoimmune conditions, and decreased abundances of protective and anti-inflammatory species, at various time points before CD onset.
- Several other species/pathways/metabolites had not been previously reported and may be CD-specific, including increased abundance of D invisus, Parabacteroides sp., and L bacterium, species previously linked to pre-type 1 diabetes, Behcet disease, and obesity.
- Species and strains decreased in abundance included S thermophilus, F prausnitzii, and C clostridioforme, previously described as acting as a probiotic, blocking release of inflammatory cytokines, and related to butyrate production.
- Porphyromonas sp., specifically strain 31_2, was increased in abundance at all time points except −18 months; other Porphyromonas sp., have previously been reported to activate the innate immune system, impair the gut barrier, and be implicated in development and severity of rheumatoid arthritis.
- Most altered pathways were differentially abundant ≤ 15 months before CD onset, suggesting potential early epigenetic influence of the gut microbiome on key immune functions, including those modulating the gluten tolerance/immune response balance.
- Study limitations include small sample size, limiting statistical power, and use of fecal samples, which may not accurately reflect small intestinal microbiota.
Experts Weigh In
When reached for comment, William Balistreri, MD, said, “This is another nice piece of work from Dr Fasano. While the numbers are quite small, their approach is unique and highly innovative.”
Balistreri is the Dorothy M. M. Kersten Professor of Pediatrics at Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio.
“If the results are further validated — that there are indeed microbial species, pathways, and metabolites for which the abundance is significantly altered before the onset of celiac disease — we will have a window of opportunity to intervene. It is always best to prevent than commit to long, arduous therapy,” he told Medscape Medical News.
Armin Alaedini, PhD, said this is “an important proof-of-concept study that sets the tone and serves as a guide for future investigations on the relevance of gut microbiome in the loss of gluten tolerance.”
Alaedini is a celiac disease researcher with Columbia University, in New York, New York.
“Important strengths of this work include its prospective longitudinal design, the metagenomic and metabolomic analysis of fecal samples to provide strain-level differences and more functional characterization (as opposed to the more limited 16S rRNA analyses in earlier studies), and many sampling points over a much longer period in comparison with prior studies,” he told Medscape Medical News.
“Because of the study’s design, the researchers were able to attempt linking microbial species and metabolites with potential disease mechanistic pathways, mainly associated with inflammation and autoimmunity, which can be further investigated for potential therapeutic and diagnostic relevance, especially in the context of preventing the loss of gluten tolerance and onset of autoimmunity in celiac disease,” Alaedini added.
He said the comparative differences in the abundance of certain strains immediately before disease onset is “intriguing, as certain similar changes have been found in previous work in the context of celiac disease and other autoimmune disorders, further documenting the significant immunomodulatory impact of these particular bacteria.”
Alaedini cautioned that, given the “tremendous diversity and oscillation in the human gut microbiome, the number of subjects in this study (10 in each arm) is too small to make firm conclusions regarding the potential biomarker value and pathogenic relevance of the generated data at this point, but this body of work still provides an excellent basis and a roadmap upon which future larger studies can be built.”
The research was partially supported by funding from the National Institutes of Health, the Nutrition Obesity Research Center at Harvard, and the Thrasher Research Fund. Leonard serves as a consultant to 9 Meters Biopharma and Anokion and performs sponsored research with Glutenostics LLC. Fasano is a stockholder at Alba Therapeutics, serves as a consultant for Inova Diagnostics and Innovate Biopharmaceuticals, is an advisory board member for Axial Biotherapeutics, and has a speaker agreement with Mead Johnson & Company. Alaedini and Balistreri have disclosed no relevant financial relationships.