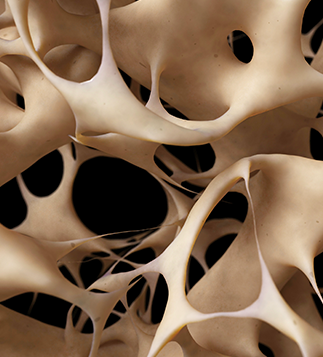
Osteoporosis Diagnosis Does Not Warrant Celiac Disease Screening
- Lorraine L. Janeczko, Reuters Health News, Top News in Family Medicine 1
“In this first systematic review of all studies testing for celiac disease in people with osteoporosis, we found that the overall prevalence of celiac disease was 1.6%. In other words, about 1 in 62 people with osteoporosis have celiac disease. This is more common than in the general population (about 1 in 100 people have celiac disease), but not far greater,” said Dr. Benjamin Lebwohl of the Celiac Disease Center of Columbia University College of Physicians and Surgeons in New York City.
“In other words, looking for celiac disease in this population is still like finding a needle in a haystack. It’s appropriate to do so, but we will often not find it,” he told Reuters Health by email.
As reported online July 8 in Alimentary Pharmacology & Therapeutics, the research team searched the standard medical databases for studies looking at the prevalence of CD in patients with osteoporosis.
They identified eight relevant studies including data from 3,188 people. Of these, 1.9% had CD. A weighted pooled analysis revealed biopsy-confirmed CD in 1.6% of patients with osteoporosis. Heterogeneity was moderate (I2=40.1%) and was affected by the underlying CD prevalence in the general population.
- “Although patients with diagnosed celiac disease are at increased risk of fractures, our study shows that patients with osteoporosis should not automatically be screened for celiac disease,” said senior author Dr. Jonas F. Ludvigsson of Karolinska Institutet in Stockholm. ” However,” he told Reuters Health by email, “my personal opinion is that, in a patient with osteoporosis and additional signs of celiac disease, I would still screen.”
Dr. Lebwohl explained that celiac disease is on the rise and osteoporosis is increasingly common with the aging population.
“We know that osteoporosis can be a consequence of celiac disease, and people with celiac disease have an increased risk of fractures, particularly before they start a gluten-free diet or if they have ongoing intestinal damage due to frequent gluten exposure after diagnosis,” he said.
He added that limitations of the study include the small sample sizes and the inability to evaluate the severity of osteoporosis and whether celiac disease is even more common in people with particularly severe osteoporosis.
Dr. Stephen Honig, director of the Osteoporosis Center at NYU Langone Health in New York City, told Reuters Health by phone,
- “Most providers who deal with osteoporosis have their antenna up for looking for secondary causes, and celiac disease is one such cause. In our practice, we look at certain types of patients, certainly those with GI complaints or those with some evidence of malabsorption; or when we do some basic screening tests, patients with low urinary calcium excretion might prompt us to look for celiac disease.”
“Certainly in those with very low bone densities, particularly younger patients with very low bone densities, we might include a celiac screen along with screens for a lot of other conditions that can lead to low bone density,” added Dr. Honig, who was not involved in the study. “In general however, I think that in the older postmenopausal osteoporotic population without any gastrointestinal issues, it’s probably not worthwhile to screen for celiac disease.”
Dr. Ludvigsson said that his group is now investigating the risk of celiac disease in patients with iron-deficiency anemia.