Brother & Sister – One with IBD; One with CD
- Lynn Nichols, Patient Stories, healthier.stanfordchildrens.org 1
The engine of this ride is two—count them two—severe gastrointestinal diseases, one for each child. Sometimes, mom Ranjita feels like she won the reverse jackpot.
“Only my kids can hit the top,” she quips.
You may also like: Experts Meghan Donnelly, RD and Dr. Maria Ines Pinto-Sanchez discuss the similarities and differences in how CD & IBS affect the gut on ‘A Canadian Celiac Podcast.’
Jasleen, age 7, was the first to show symptoms. Luckily, Ranjita is a nurse and her husband, Amanpreet, is a pharmacist, so they suspected that something wasn’t right from the start.
“We were on our annual trip to Disneyland and Jasleen called me and said, ‘Mom, there’s red stuff in the toilet.’ At first we wrote it off as something red she may have eaten at Disneyland, but deep down I knew something was wrong,” Ranjita says.
The family returned home to Modesto, California, and when Jasleen used the bathroom the entire toilet bowl was filled with blood. They rushed her to the local emergency room (ER) where she was diagnosed with a hemorrhoid. They returned home, but the blood didn’t stop.
The family’s pediatrician advised them to return to the ER. By now Jasleen was complaining of stomach pains. Luckily, she used the bathroom while there so the doctor could see the blood and clots that Ranjita was describing. The shock of it compelled the doctor to immediately call for an ambulance to Stanford Children’s Health.
“I was at work trying to concentrate but I was so worried. When I heard Jasleen was going to Stanford Children’s I knew her condition was serious, but I was relieved to know she would be getting the best care possible,” says Amanpreet.
Diagnosing Very Early Onset IBD
“We performed a colonoscopy and we could see her entire colon was inflamed. We diagnosed her with very early onset inflammatory bowel disease (IBD),” says Alka Goyal, MD, a pediatric gastroenterologist who specializes in treating IBD in children. “Very early onset simply means IBD that starts before the age of 6.”
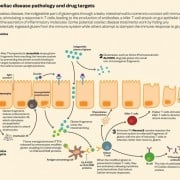
Inflammatory bowel disease (IBD) is an umbrella term for conditions that inflame the bowel. It’s caused by environmental and genetic factors that fail to maintain tolerance to the gut bacteria and activate immune system response, which attacks the gut microbiome causing further bacterial imbalance and results in the inflammation of the bowel. Common symptoms include abdominal pain, diarrhea, bloody stools, fatigue, weight loss, delayed puberty, and poor growth.
Although there is no cure for IBD, the new highly comprehensive and multidisciplinary Center for Pediatric IBD and Celiac Disease at Stanford Children’s Health helps children feel well so they can live a fulfilling life. The center approaches IBD and celiac disease from every angle, customizing a long list of treatments and therapies to care for the whole child and the whole family.
“It takes a village to care for children with IBD and celiac disease. You can’t credit just one part of the team. Everyone, from doctors, nurses, dieticians, social workers, psychologists, psychiatrists, IBD nurse coordinators, clinic and administrative staff is greatly instrumental in supporting the Basi family,” Dr. Goyal says.
Jasleen was given medicines to calm the inflammation and suppress her overactive immune system. The goal was to put her disease in remission, yet it wasn’t a simple task. She was improving, but it wasn’t lasting. Her family was desperate for a solution.
“We decided to bring her for a second opinion to Children’s Hospital of Philadelphia (CHOP). We wanted to make sure that we were on the right path and Dr. Goyal was very open to that. She said, ‘Jasleen is like a daughter to me so if there is a better therapy for her, I’m happy to work with another center to get her the right care.’ However, once the doctors at CHOP examined her and ran several tests they recommended the exact same treatment that Stanford Children’s had her on,” Ranjita says.
Yet, there was a missing link to why Jasleen wasn’t achieving remission. Dr. Goyal suspected she was eating something that was keeping her gut inflamed.
“We performed an esophagogastroduodenoscopy (EGD), or upper endoscopy scope, and I saw an increased number of allergy cells and suspected it to be due to milk allergy. Jasleen loves milk so it has been a challenge to remove it from her diet completely. They tried and it was very stressful for her. She lost interest in eating,” Dr. Goyal says.
Yet, once Jasleen was off of milk, her inflammation levels became normal. The family is vegetarian, so removing milk makes for a vegan diet. It demanded a slew of dietary changes, which were facilitated by the IBD Nutritional Therapies team, one of the most robust programs of its kind in the West.
“Before testing for lactose intolerance, doctors were thinking they might have to remove parts of Jasleen’s colon if her inflammation markers didn’t drop. It was terrifying. But then her levels dropped from 1000 to 49—such a drastic change that even Dr. Goyal couldn’t believe it,” Amanpreet says. “The diet changes and the medication were working, and it was such a relief.”
Spending time in the hospital and limiting a 6-year-old’s diet wasn’t easy, but Jasleen’s parents did everything right. They empowered Jasleen to advocate for herself and gave her permission to cry when she was scared, like with the initial poke for infusions.
“We make little compromises with her. She loves soda, so if I want a soda, I ask her if it’s okay if I have one. If she says no, I don’t. I tell my kids, if you want me to eat the same diet you have to, I will,” Amanpreet adds. “It’s only fair.”
Next up, Celiac Disease
If that wasn’t enough for the family to handle, Jeevan, age 12, was diagnosed with severe celiac disease at about the same time. Ranjita noticed that Jeevan hadn’t grown or gained weight. His shirt, shoe, and pants sizes hadn’t changed in about two years.
“I felt like he had been a size 8 forever,” Ranjita says. “I took him to an endocrinologist and they thought it was a thyroid problem because his thyroid levels were off the charts. Yet medications were not working.”
Next, the doctor performed a GI panel. Sure enough, Jeevan came back positive for celiac disease. Ranjita returned to Stanford Children’s Health. Celiac disease demands a strict gluten-free diet, which meant another major adjustment to the family’s eating habits. Without dairy, meat, wheat and other gluten-containing grains, it felt like there wasn’t a lot left to eat.
“When a child is diagnosed with a gastrointestinal disease it is a shock to families. I can’t imagine what it’s like to have two children with intestinal disease. Their whole lives have been turned upside down,” Dr. Goyal adds.
Venus Kalami, MNSP, RD, CSP, an expert nutritionist in GI disorders, guided an overwhelmed Ranjita on how to use alternative flours in her cooking and baking. Yet, Jeevan still didn’t gain weight and his inflammatory markers for gluten still remained high.
“We felt like we were hitting rock bottom with both kids struggling at the same time. To cope, we turned to religion. We took the kids to India to the Golden Temple to ask for guidance,” Ranjita says. “Having a strong faith, helps. Today, we meditate together for 30 minutes every day.”
The Celiac Disease Program team had some digging to do. Mom was doing everything right to exclude gluten from Jeevan’s diet, so they suspected cross contamination in the family’s cooking methods. The care team requested that Ranjita give them a tour of her kitchen via video chat. They asked about where she made food, how she stored it, and what pots and pans she used. It came down to cookware. Now, Ranjita has one set for Jeevan and one for Jasleen.
“Shortly after, they ran his labs again and there was no sign of gluten. After that, he grew like 5 inches and he gained about 20 pounds. It was like his body was waiting to grow,” Ranjita exclaims.
“He gained weight so fast and slept so much better. It was like a miracle,” Amanpreet adds.
Life goes on, with support
Besides nutritional support, the family has also received a ton of help from the robust psychosocial services team within the Pediatric IBD and Celiac Disease Center. The psychosocial team has provided family therapy, which has helped manage Ranjita’s stress and lower Jasleen’s anxiety about her disease. In addition, they connected the parents with other families of children with IBD and celiac disease. They also helped the family overcome roadblocks with work and school, including helping to put in place 504 learning plans for the kids. California law requires schools accommodate medical conditions, such as allowing the kids to take a break when they don’t feel well, turn down school food, and go to the bathroom when needed.
“We reached out to the kids’ schools to educate their teachers and support staff on their diseases. It’s stressful enough to learn, let alone do it while managing discomfort and pain,” says Garret Forshee, LCSW. “Working exclusively within the celiac and IBD center, I deeply understand what these families are facing and I can anticipate their needs. I have such respect for Ranjita and Amanpreet. They are doing an amazing job juggling the needs of their kids.”
The family is settling into a routine. The injectable medication, along with changes in diet and support for anxiety, have worked for Jasleen and she has felt good for a year now. And Ranjita can’t keep up with buying clothing to match Jeevan’s continued growth.
“It feels better to be on the other end. We are at the stage where we can joke around about it a bit. Ranjita even volunteered to talk with parents of newly-diagnosed children,” Amanpreet says. “We’re guided by our strong faith and inspired by how our parents and family have rallied behind us, and we are grateful for all of the support we’ve gotten from Dr. Goyal and her team—she’s so responsive and wonderful.”
The family receive regular follow-up visits with the medical team and meets with their dietitian regularly via telehealth to gain support and stay on track with diet demands. Otherwise, life is finally calming down.
“Ranjita is such a dedicated mom. She’s got one foot squarely in the reality that her kids need to be kids and another foot in our world, wanting gold standard care for them,” says Venus Kalami, MNSP, RD, CSP. “We’re here to serve our patients, but they serve us, too. We are filled up by parents like Ranjita and Amanpreet who are connected and dedicated to their kids.”
The parents are grateful that Stanford Children’s Health has one comprehensive center with multiple experts under one roof to care for their kids. They couldn’t be more pleased that the kids see the same doctor, and they are able to coordinate visits and tests.
“It’s convenient, but more importantly, I really feel like they know my family and understand our history and our beliefs,” Ranjita says.
Despite it being the place where their tipsy-turvy, head-spinning journey began, the family returned to Disneyland last fall.
“It was scary, and we had some post-traumatic stress, but we had a great time,” Ranjita concludes.