Abnormal Biopsy Alone Does not Diagnose Celiac Disease
by Carol Semrad, MD, Abnormal Biopsy Alone Does Not Diagnose Celiac Disease, CdC_Newsletter_2016_Issue01*
“Often when I am in clinic, a Gastroenterology Training Fellow will inform me that another patient has “biopsy proven” celiac disease. Each time, I question the fellow: “Do you mean this patient had a small bowel biopsy that was abnormal, started a gluten-free diet, and then repeat biopsy returned to normal?” This was how the diagnosis of celiac disease was made before modern day antibody testing combined with an abnormal duodenal biopsy. The fellow’s answer is usually that only one biopsy was obtained at the time of diagnosis. My next question is, “was celiac antibody testing positive”? Why is antibody testing necessary? Why is an abnormal duodenal biopsy alone not sufficient to diagnose celiac disease? Because the type of inflammation found in celiac disease (increased lymphocytes at the surface and underneath the intestinal lining with associated shortened villi ) is found in other small bowel diseases or injury as well.”
“Other causes, particularly with milder inflammation, include acid injury, bacterial overgrowth, Crohn’s Disease, and an entity that we are seeing more of in our increasingly global economy, tropical sprue.”
“More problematic is the older adult population. Many have been incorrectly diagnosed with celiac disease by small bowel biopsy alone, only to find out the real cause was a drug, such as olmesartan (for high blood pressure), mycophenolate (an immunosuppressant), or a chemotherapy agent (for cancer). When a pharmaceutical agent causes the inflammation, a gluten-free diet will not cure symptoms but stopping the drug will.”

Celiac disease – what it is, what is isn’t. gfjules.com
“Additional pitfalls of small bowel biopsy include distorted villi due to glands beneath the lining of the duodenal bulb (entry way from stomach to duodenum), inadequate number of biopsies taken for interpretation, and poor orientation while making the biopsy slides. In addition, pathologists may miss-diagnose celiac disease if they do not consciously look for other causes such as infection (giardia, cryptosporidium) or loss of plasma cells seen with immune deficiency states.”
“In these more difficult situations, it may take an expert gastrointestinal pathologist to accurately interpret the biopsy findings. Remember, duodenal (small bowel) inflammation is found with active celiac disease but not all that is inflamed in the duodenum is celiac disease. This is why celiac antibody studies, duodenal biopsy, and sometimes genetic testing for the HLA DQ2 or DQ8 risk alleles are needed to make a secure diagnosis of celiac disease while the patient is eating gluten.”
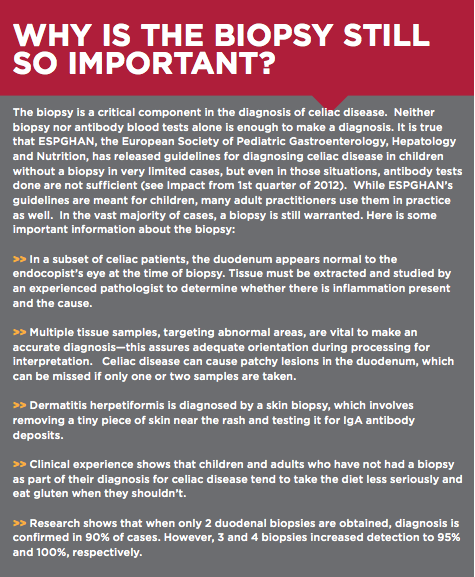
“The biopsy is a critical component in the diagnosis of celiac disease. Neither biopsy nor antibody blood tests alone is enough to make a diagnosis. It is true that ESPGHAN, the European Society of Pediatric Gastroenterology, Hepatology and Nutrition, has released guidelines for diagnosing celiac disease in children without a biopsy in very limited cases, but even in those situations, antibody tests done are not sufficient (see Impact from 1st quarter of 2012). While ESPGHAN’s guidelines are meant for children, many adult practitioners use them in practice as well. In the vast majority of cases, a biopsy is still warranted. Here is some important information about the biopsy:
- In a subset of celiac patients, the duodenum appears normal to the endocopist’s eye at the time of biopsy. Tissue must be extracted and studied by an experienced pathologist to determine whether there is inflammation present and the cause.
- Multiple tissue samples, targeting abnormal areas, are vital to make an accurate diagnosis—this assures adequate orientation during processing for interpretation. Celiac disease can cause patchy lesions in the duodenum, which can be missed if only one or two samples are taken.
- Dermatitis herpetiformis is diagnosed by a skin biopsy, which involves removing a tiny piece of skin near the rash and testing it for IgA antibody deposits.
- Clinical experience shows that children and adults who have not had a biopsy as part of their diagnosis for celiac disease tend to take the diet less seriously and eat gluten when they shouldn’t.
- Research shows that when only 2 duodenal biopsies are obtained, diagnosis is confirmed in 90% of cases. However, 3 and 4 biopsies increased detection to 95% and 100%, respectively.”
“Remember, duodenal (small bowel) inflammation is found with active celiac disease but not all that is inflamed in the duodenum is celiac disease. This is why celiac antibody studies, duodenal biopsy, and sometimes genetic testing for the HLA DQ2 or DQ8 risk alleles are needed to make a secure diagnosis of celiac disease while the patient is eating gluten.”
- https://www.cureceliacdisease.org/wp-content/uploads/CdC_Newsletter_2016_Issue01_FINAL.pdf
- Carol Semrad, CdC_Newsletter_2016_Issue01
Past editions impact magazine • Facebook • Twitter
Help Fund the Cure – The Celiac Disease Centre depends on private donors like you!
“The University of Chicago Celiac Disease Center is dedicated to finding a cure for celiac disease. As we focus on research toward a cure, we also strive to raise awareness and diagnosis rates through education and advocacy. Our work is entirely funded by private donations. Until we are able to raise enough funds for an endowment, growing and sustaining our research and much-needed programs and services require us to raise new funds each year.”
“What your donation supports – The University of Chicago Celiac Disease Center, a 501(c)(3) organization within The University of Chicago, is completely funded from private donations. When you contribute to The Celiac Disease Center, you help support vital research projects, including our efforts to find a cure as well as important programs and services, including the Gluten-Free Care Package Program, the Celiac Disease Answer Bank, the Annual Celiac Education Day and the Preceptorship Program”
“The University of Chicago Celiac Disease Center, a 501(c)(3) organization within The University of Chicago, is completely funded from private donations. When you contribute to The Celiac Disease Center, you help support vital research projects, including our efforts to find a cure as well as important programs and services, including the Gluten-Free Care Package Program, the Annual Celiac Education Day and the Preceptorship Program”
“The Center is pleased to be able to accept donations online. Simply click on DONATE NOW. After you donate, you will receive confirmation via email. If you prefer to send a check, kindly make it payable to The University of Chicago Celiac Disease Center, and mail to:
- The University of Chicago Celiac Disease Center
- 5841 S. Maryland Avenue, Mail Code 4069
- Chicago, IL 60637
Corporate Matching – for information on programs or institutional donations, please call773-702-7593.
Endowment – the Center is working to establish a $5 million endowment for The Celiac Disease Center.”