Celiacs Not at Higher Risk of Contracting COVID-19
 Be assured! Results of cross-sectional study to evaluate whether patients with self-reported CeD are at an increased risk of contracting COVID-19 are in!
Be assured! Results of cross-sectional study to evaluate whether patients with self-reported CeD are at an increased risk of contracting COVID-19 are in!
- Clinical Gastroenterology and Hepatology 1
INTRODUCTION
The World Health Organization declared coronavirus disease-2019 (COVID-19) a global pandemic in March 2020. Since then, there are over 34 million cases of COVID-19 leading to over 1,000,000 deaths worldwide.
Numerous studies suggest that celiac disease (CeD), a chronic immune-mediated gastrointestinal condition triggered by gluten, is associated with an increased risk of respiratory infections 1-3.
However, how it relates to the risk of COVID-19 is unknown. To address this gap, we conducted a cross-sectional study to evaluate whether patients with self-reported CeD are at an increased risk of contracting COVID-19.
RESULTS
- A total of 18,022 participants completed the survey.
- From them, 10,737 had self-reported CeD; they were older (mean 32 vs 41 years; p<0.01) and had a higher proportion of females when compared to the control group (85% vs 80%; p<0.001).
- CeD was confirmed by duodenal biopsy in 7506 patients (69.9%).
- Thirty-two percent of CeD had persistent symptoms.
- A strict GFD was reported by 65.7% and 3.9% of CeD patients and controls, respectively.
- A greater proportion of CeD had co-morbidities including respiratory (6.6% vs 3.7%; p<0.001), cardiac (3.5% vs 1.9%; p<0.001) and diabetes (3.8% vs 2.5%; p<0.001) compared with controls.
- CeD patients were significantly less likely to have been tested for COVID-19 (4.5% vs 6.6%;p<0.001) and being exposed to COVID-19 (1.6% vs 4%;p<0.001) compared with controls.
- Out of 940 participants tested for COVID-19, 8.7% reported a positive test.
- There was no difference in the odds of having a positive test for COVID-19 in CeD compared with controls (9.4% vs 8.1%; OR:1.18; 95%CI=0.75-1.84).
- Subgroup analyses within the CeD group showed no difference in the odds of contracting COVID-19 in patients with and without biopsy confirmation of CeD (9% vs 10%;p=0.65); symptomatic vs not-symptomatic CeD (11% vs 7%;p=0.13); or those adopting a strict-GFD vs not-strict-GFD (9% vs 10%;p=0.74).
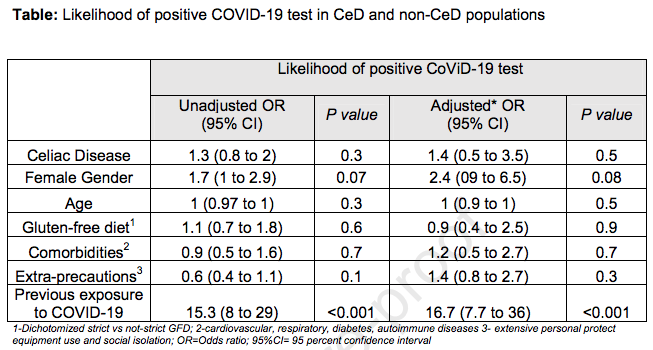
Twenty-eight percent of CeD reported taking extra safety precautions for COVID-19; however, this did not change the likelihood of a positive COVID-19 test. Exposure to a COVID-19 contact was the only factor increasing the odds of a positive test (Table).
DISCUSSION
To our knowledge, this is the first large-scale study to examine risk of COVID-19 in CeD compared to non-celiac population. We found that patients with CeD had a similar odds of contracting COVID-19 when compared with the controls. The presence of comorbidities, which was identified as important predictor of morbidity and mortality associated with COVID-19 5, were more frequent in CeD than controls. However, this did not result in higher odds of a positive COVID-19 test in CeD. We hypothesized that adopting a strict-GFD and having fewer symptoms 8 would decrease the odds of contracting COVID-19 in CeD; however, this was not confirmed in our analyses. It is of common knowledge 6 that previous exposure to someone with COVID-19 increases the risk of contracting COVID-19, and this was confirmed in our study. However, CeD were less exposed to COVID-19 than controls, which may have influenced the results. We acknowledge the presence of limitations related to the design of our study, which used a web-based survey for data collection, and therefore, the source of information provided by participants cannot be confirmed. The study was not designed to assess differences in COVID-19-related severity outcomes, and it is our hope that the ongoing international SECURE-Celiac registry (www.covidceliac.org), will further address this.
- In conclusion, patients with CeD have similar odds of contracting COVID-19 and may not need to take additional precautions to prevent exposure aside from that recommended to the general public. Longitudinal studies employing repeated measurements will contribute to a better understanding on whether the risk of contracting COVID-19 in CeD changes over time.
METHODS
This study was conducted between March and June 2020. Participants of all ages with a self-reported CeD diagnosis and those without CeD from different countries including Argentina, Australia, Canada, Italy, Mexico, New Zealand, Spain, Uruguay and the United States were recruited through local CeD associations, electronic newsletters and social media. Participants completed a web-based survey consisting of 41 items which was translated into Spanish and Italian using the approach proposed by Mallinckrodt 4 . Data on demographics, gluten-free diet (GFD), symptomatology, COVID-19 testing were collected using RedCap®.
Statistical analyses were carried-out using IBM-SPSS v.25. Continuous and categorical variables were compared using the Mann-U-Whitney and χ 2 test. Logistic regression was performed to assess the impact of different factors on the likelihood of reporting a positive COVID-19 test (dependent variable). Independent variables included CeD diagnosis, age, gender, comorbidities, GFD adherence, extra precautions and previous Journal Pre-proof COVID-19 exposure. The unadjusted and adjusted ORs were reported with their 95% confidence intervals.
J. Zhen, J.P. Stefanolo, M.P. Temprano, S. Tedesco, C. Seiler, A. Caminero, E. de-Madaria, M. Montoro Huguet, S. Vivas, S. Niveloni, P. Bercik, E. Smecuol, L. Uscanga, E. Trucco, V. Lopez, C. Olano, P. Mansueto, A. Caroccio, P.H. Green, A.S. Day, J.A. Tye-Din, J.C. Bai, C. Ciacci, E.F. Verdu, B. Lebwohl, M.I. PintoSanchez
REFERENCES
1. Mårild K, Fredlund H, Ludvigsson JF. Increased risk of hospital admission for influenza in patients with celiac disease: a nationwide cohort study in Sweden. Am J Gastroenterol. Nov 2010;105(11):2465-73.
2. Simons M, Scott-Sheldon LAJ, Risech-Neyman Y, et al. Celiac Disease and Increased Risk of Pneumococcal Infection: A Systematic Review and MetaAnalysis. Am J Med. 2018;131(1):83-9.
3. Ludvigsson JF, Wahlstrom J, Grunewald J, et al. Coeliac disease and risk of tuberculosis: a population based cohort study. Thorax. 2007;62(1):23-8.
4. Mallinckrodt B, Wang C.Quantitative methods for verifying semantic equivalence of translated research instruments: A chinese version of the experiences in close relationships scale. J Counsel Psychol 2004;51:368-79.
5. Zheng Z, Peng F, Xu B, et al. Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J Infect. 2020;81(2):e16-e25
6. Emmi G, Bettiol A, Mattioli I, et al. SARS-CoV-2 infection among patients with systemic autoimmune diseases. Autoimmun Rev. 2020;19(7):102575.
7. Wiersinga WJ, Rhodes A, Cheng AC, et al. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. JAMA. 2020;324(8):782-93.
8. Emilsson L, Lebwohl B, Green PH, et al. Mucosal healing and the risk of serious infections in patients with celiac disease. United European Gastroenterol J. Feb 2018;6(1):55-62.
PII: S1542-3565(20)31398-7
DOI: https://doi.org/10.1016/j.cgh.2020.10.009
Reference: YJCGH 57547
1 https://www.cghjournal.org/article/S1542-3565(20)31398-7/pdf