Elevated Liver Enzymes in Celiac Disease Often Normalize with Gluten-Free Diet
 Four in 10 patients with celiac disease (CD) have abnormal liver function tests (LFTs) at diagnosis, but they generally normalize with treatment according to the American Journal of Gastroenterology , (7 July 2015) | doi:10.1038/ajg.2015.192
Four in 10 patients with celiac disease (CD) have abnormal liver function tests (LFTs) at diagnosis, but they generally normalize with treatment according to the American Journal of Gastroenterology , (7 July 2015) | doi:10.1038/ajg.2015.192
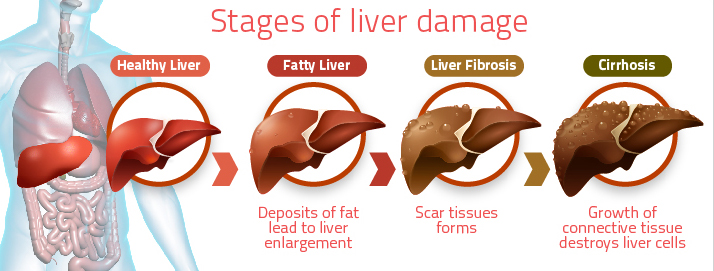
CD is known to be associated with several disorders of the liver, according to Dr. Daniel Leffler of Beth Israel Deaconess Medical Center in Boston and colleagues. Up to half of adults and children with CD have elevated LFTs when they are diagnosed, the researchers note. Guidelines call for LFTs at diagnosis and then annually.
“However, not all recent studies have shown this high prevalence of LFT abnormalities in CD patients, casting some doubt on the need for routine liver evaluation in this population,” Dr. Leffler and his team wrote.
To investigate the prevalence of abnormal LFTs in U.S. CD patients, and the effect of a gluten-free diet on LFTs, the researchers looked at data on 463 adults with biopsy-confirmed celiac disease and matched controls, plus 7789 people participating in the 2009-2010 National Health and Nutrition Examination Survey (NHANES).
As reported online July 7 in the American Journal of Gastroenterology, aminotransferase levels were significantly higher in the celiac patients (ALT, 36.7 vs. 26.4IU/L and AST, 34.3 vs. 25.8IU/l, P<0.001 for both). Before treatment, 40.6% of the CD patients had elevated LFTs, compared with 16.6% of matched controls. In the NHANES cohort, 36.7% of people with CD had abnormal LFTs, versus 19.3% of those without CD.
Among patients who followed a gluten-free diet for a mean of 1.5 years, nearly 80% (132/168) of those with abnormal LFTs at diagnosis had normalized. When follow-up was extended to an average of nearly four years, however, only about 60% (100/168) had persistently normal liver function.
“These data support the screening for LFT abnormalities in all newly diagnosed CD individuals,” Dr. Leffler and his team wrote. “Strict adherence to a (gluten-free diet) can reduce LFT abnormalities within a year and patients with sustained LFT abnormalities despite a (gluten-free diet) should be evaluated for coexisting liver diseases. A ‘treat-first then re-evaluate’ approach should be initially considered by clinicians instead of initial, extensive investigation for chronic liver disorders.”
From the Canadian Celiac Association, Related Conditions, Liver Abnormalities:
“CD affects around 1% of the general population. Liver abnormalities are a common extraintestinal manifestation in patients with CD. The liver injury in CD has a wide spectrum ranging from mild hepatic abnormalities to severe liver disease. The mechanisms underlying liver injury in CD are poorly understood; however, a GFD is an effective medical therapy for most patients with CD and liver injury. The association of CD with other chronic liver disorders (for example, autoimmune liver disorders) is well established. The effect of a GFD on the progression of liver diseases associated with CD is less clear. Finally, although there are many gaps in our understanding of how CD and the liver interact, it is possible to suggest a rational approach to the investigation and clinical follow-up of the liver abnormalities commonly associated with CD.”